Lung cancer treatments are complex, lengthy and can cause debilitating side effects. And because a treatment may not be effective for a particular patient, it is important to learn early on whether or not it is working so that alternative cancer fighting tools can be employed where appropriate. Analysis of blood samples using liquid biopsy can monitor cancer cell destruction as early as four weeks into treatment, but current approaches are ineffective for non-small cell lung cancer (NSCLC).
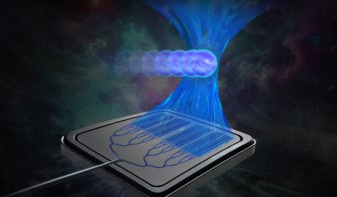
This may change with the development of a novel ultrasensitive graphene oxide (GO) microfluidic chip by researchers at the University of Michigan. The team’s “GO chip” can isolate and capture enough circulating tumour cells (CTCs) in the blood of NSCLC patients for laboratory analysis. CTCs are early signs of metastasis and strong predictors of future progression, but their low concentration in the blood – 10 to 100 CTCs/ml, compared with a background of 108 white blood cells – makes their detection and analysis challenging.
Current tests for detecting CTCs in blood capture a single type of protein on the cell surface that’s infrequent in lung cancers. Instead, the GO chip is designed to capture a wider range of surface proteins specific to lung tumours. The chip uses immunoaffinity, antibodies against these CTC surface proteins, to capture and immobilize them on functionalized gold nanoposts as blood is pushed through the chip’s channels during testing.
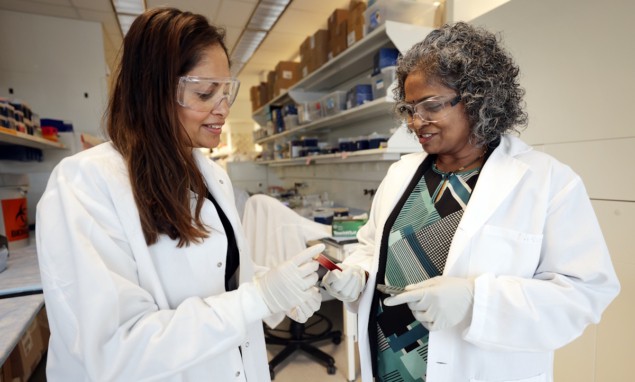
Principal investigators Sunitha Nagrath and Shruti Jolly and their colleagues investigated the GO chip’s effectiveness at measuring CTCs in 26 patients with stage III NSCLC. They recorded measurements throughout the patients’ treatment cycles – which comprised chemoradiotherapy followed by 12 months of anti-PD-L1 immunotherapy – following up the patients for an average of 21 months. They also performed molecular characterization to develop CDC signatures that predict which patients have a shorter or longer progression-free survival.
For the study, the researchers analysed blood samples at six time points: pre-treatment, during and after chemoradiotherapy (weeks 1, 4 and 10) and during immunotherapy (weeks 18 and 30). They used two GO chips for each patient blood sample, one for CTC analysis and the other for RNA extraction of captured CTCs.
Writing in Cell Reports, Nagrath and Jolly report that CTCs decreased significantly during treatment for all patients. They observed a significant decrease in CTC counts from baseline following the first chemoradiation treatment, as well as at week 10 with the commencement of immunotherapy and at week 30. However, there was no correlation between the gross tumour volume and absolute CTC quantity throughout the duration of the blood testing.
Patients with a decrease in CTCs of less than 75% between baseline and week 4 had a shorter progression-free survival, with a mean time before progression of seven months. Patients with a decrease of 75% or greater were progression-free throughout the 21-month long study. This finding demonstrates the potential for using CTCs as an early predictor of progression.
The researchers also conducted mRNA analysis using the microarrays to compare gene expressions. Gene expression changes over time indicated that CTCs shed by tumours that survive chemoradiation may be more metastatic and more aggressive.

Personalized lung cancer radiotherapy proves safer, more effective
“We have now shown that CTCs are potential biomarkers to monitor and predict patient outcomes in patients with stage III NSCLC,” says Jolly in a press statement. “Currently, there is typically a wait of weeks to months before we can fully assess the effectiveness of cancer treatment. However, with this chip, we may be able to sidestep prolonged, ineffective therapy and quickly pivot to alternatives, thus saving patients from needless side effects. This technique has the potential to shift cancer diagnostics, moving from a delayed single assessment to a more continuous surveillance, and facilitating the delivery of personalized cancer treatment.”
Nagrath tells Physics World that the study results could also be relevant to other solid tumours. “We are currently testing the utility of GO chip in other solid tumours, such as bladder cancer, to identify the more aggressive disease,” she says. “We are also planning to conduct a larger cohort study in the future to confirm our initial findings.”