Introducing automated tools into the treatment planning process has enabled the clinical team at the UK’s Castle Hill Hospital to improve consistency while also achieving significant time savings
Intelligent software solutions have become a crucial tool for stretched clinical teams to provide the best possible care to cancer patients, particularly those that require more complex treatments using higher radiation doses. Software systems with built-in artificial intelligence can automate repetitive tasks, enhance the information that can be extracted from CT simulators, and ensure consistency of care across an increasing number of cases.
At Castle Hill Hospital in Cottingham, UK, which treats several hundred patients every month with its six linear accelerators, intelligent software has been deployed across the entire treatment planning process. “We try to make use of every tool at our disposal, whether it’s simple decision trees or commercial software that makes our work easier and more efficient,” says Carl Horsfield, principal physicist at Hull University Teaching Hospitals NHS Trust. “Like many treatment centres we are short of staff when compared to national models, and we use software to help us deliver high-quality care.”
Right at the start of the process, automated software on the CT simulators – the SOMATOM go.Open Pro from Siemens Healthineers – maintains the sensitivity of the images by modulating the radiation dose to match the size of the patient. The scanners are also equipped with a smart algorithm, called Direct i4D, that improves the quality of time-resolved images that are used to capture the breathing motion of patients with lung cancer. Normally these 4D CT scans only produce accurate images when regular breaths are taken during the acquisition time, typically around two minutes, but that is rarely the case for patients with lung conditions.
“Lung patients are often complex and problematic at CT, and I have spent a great deal of time attending scans to assess whether the images for 4D lung patients are clinically suitable,” says Horsfield. “With this smart algorithm the scan parameters adapt to the patient’s breathing in real time, which makes the radiographers much more confident in the acquisition when the breathing pattern is irregular.”
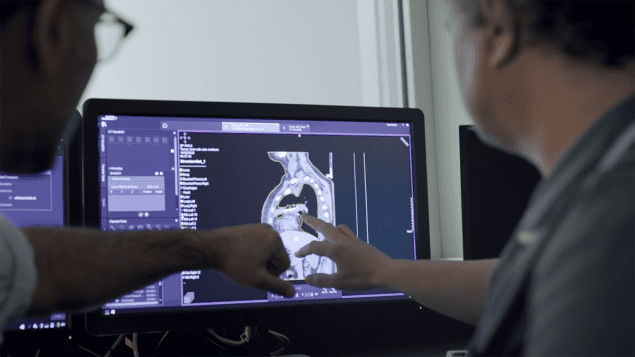
Even more significant time savings can be achieved by using an AI-powered solution embedded in the CT scanner, called DirectORGANS, that combines the image data with a deep-learning algorithm to automatically contour the patient’s critical organs. Such automatic contours are generated for every radical patient who is treated at Castle Hill, avoiding the need for a clinician to draw every structure by hand. In congested treatment sites, like the head-and-neck, that can reduce the time taken by an hour or more. “Saving time for our clinicians is paramount, and autocontouring is a fantastic way to ensure they are not repeating simple tasks for multiple patients,” comments Horsfield.
Importantly, the accuracy of the automatic contours – and therefore the amount of time that can be saved – depends on the quality of the input data. DirectORGANS offers a key advantage here, since it captures a bespoke dataset from the CT scan that has been optimized to generate the best results from the deep-learning algorithm. “Many autocontouring tools are hosted in the cloud, which means that they only have access to the scan that has been configured for the needs of the clinical team,” explains Horsfield. “One of the reasons we like DirectORGANS is that it makes its own reconstruction, setting the parameters on the acquiring scanner to match the way the organs should be made.”
The software generates accurate contours for many common organs-at-risk, including the lung, prostate, bladder and spinal canal. Once created, the patient’s clinician at Castle Hill always reviews the structures, edits them as needed, and manually delineates the tumour. Crucially, the clinician must also approve the final set of contours before they are used for treatment planning. “A clinician still needs to make sure that the contours produced by the algorithms are fit for purpose,” says Horsfield. “We also prompt them to provide feedback on the quality of the organs, which provides us with some internal quality assurance.”
While the initial version of the software included 30 or 40 pre-loaded structures, the latest release has improved the coverage and accuracy still further. One key advance, for example, is the ability to automatically contour the lymph node chains, normally a manual and painstaking task. “For prostate patients where there is risk of nodal infiltration, the clinicians need to work their way all the way from the prostate across the sacrum to the end of the local lymph-node chain,” explains Horsfield. “Having automated contouring for those kinds of structures will be a massive saving for them, even on the occasion when some editing is required.”
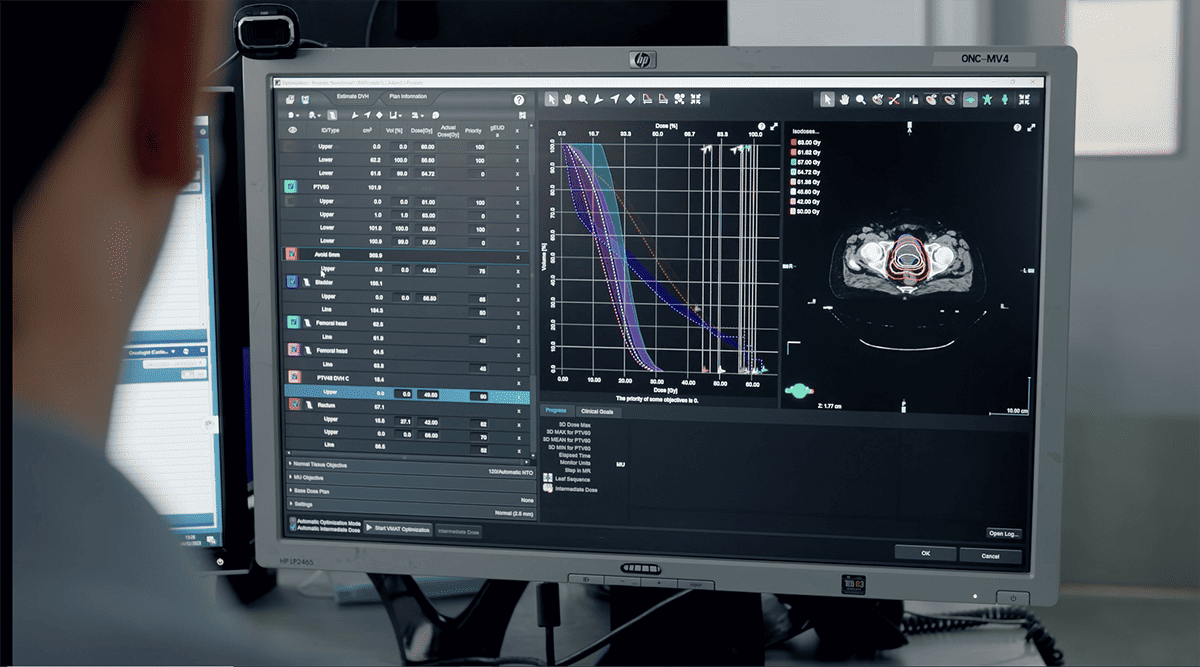
Meanwhile, a number of automated tools are also built into the team’s treatment planning system, Varian’s Eclipse. One that has proved particularly useful for the Castle Hill team is RapidPlan, a knowledge-based solution that uses a model created from previous cases to generate a personalized treatment plan for a new patient. “It’s a tool that helps us to determine what is achievable for each patient, particularly for more complicated cases where the location of the organs-at-risk might compromise the coverage of the target,” says Horsfield. “We have class solutions for our treatment plans as starting points, but it’s smarter than that because it is specific to the anatomy of each patient.”
This knowledge-based approach has proved particularly beneficial for new staff members, and has also improved the consistency and quality of the plans produced across the whole team. “Someone who has been with us for six months might not create a plan of the same standard as one of our more experienced team members,” says Horsfield. “Augmenting their knowledge with these intelligent tools allows them to access that experience and standardizes the quality of the plans we produce.”
As with any machine-learning approach, the quality of the predictions depends on the training data used to create the model. At Castle Hill the team has used its own cases to develop models for four treatment sites – the lung, head-and-neck, oesophagus and prostate – with several others now being developed to realize further time savings for the planning team. “One of the big difficulties with treatment planning is knowing when to stop,” says Horsfield. “RapidPlan provides the reassurance that you have found an optimal solution for that patient, and that there’s less benefit to spending additional time questioning your choices.”
The Eclipse treatment planning system also provides an interface for adding bespoke tools to the planning process. As an example, the team at Castle Hill has created an automated tool for creating optimization structures, which constrain the solutions produced by the treatment planning system by defining particular areas that should not be targeted with radiation. “We’ve made about 15 different protocols to create these avoidance and optimization structures,” says Horsfield. “They are all simple operations, but we realized that they were being done manually for nearly every treatment plan. It’s been really empowering to be able to create our own tools for making our processes more efficient.”
Such efficiency savings are particularly critical at a time when treatment centres like Castle Hill are dealing with the fallout from the COVID-19 pandemic. With a huge influx of patients and a shortage of healthcare professionals, intelligent tools that can automate at least some of the treatment planning process is helping ongoing efforts to work through the backlog. “Our capacity before COVID was to produce 40 plans per week, and now the whole team is making a big push to increase that to 50,” says Horsfield. “Every efficiency we can achieve by automating our processes is helping us to make headway against our recovery plan, while also ensuring that we continue to produce high-quality plans for every patient we treat.”




