A new study on the mechanical stability of bonds between the spike protein on the SARS-CoV-2 virus and its receptors on human cells during infection has revealed differences in the binding stability of viral variants such as Omicron and Delta. The finding, from researchers in the Netherlands, Germany and the US, could help explain why some variants spread more quickly than others.
SARS-CoV-2, the virus responsible for COVID-19, contains four structural proteins: envelope (E); membrane (M); nucleocapsid (N); and spike (S). The M, E and S proteins are vital for assembling and forming the virus’ outermost layer, including the mechanisms by which the virus enters host cells. The N protein, meanwhile, encapsulates the virus’ genetic information.
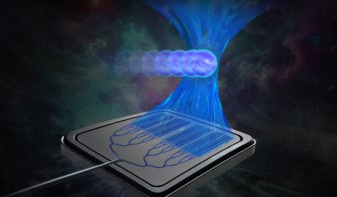
Magnetic tweezers technique
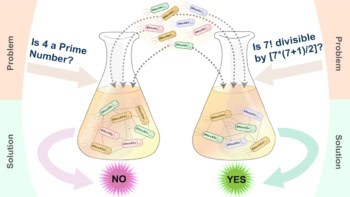
In the new work, a team led by physicist Jan Lipfert of Utrecht University in the Netherlands used a highly sensitive technique called magnetic tweezers to study the biomechanical properties of chemical bonds in the SARS-CoV-2 virus under conditions that mimic those of the human respiratory tract. Their assay uses a protein construct that combines the receptor-binding domain of the virus (essentially the tip of the spike protein) and the extracellular domain known as ACE2 (the virus’ cellular receptor and a key entry point into human cells). These two components are connected via a flexible peptide linker.
“In addition, our construct features peptide tags to attach it with one end to a surface and with one end to a small magnetic bead,” explains Lipfert. “Using this construct, we can apply precisely calibrated forces to the interface of the virus protein bound to its cellular receptor.”
Since the two binding partners are connected with a linker, they can rebind after the bond breaks, he adds. “This allows us to study the interactions over and over again, at different forces.”
Stronger binding
The researchers found that while all the major SARS-CoV-2 variants (including Alpha, Beta, Gamma, Delta and Omicron) have a higher binding affinity to human cells than the original strain, the binding of the Alpha variant is especially mechanically stable. This could explain why it spread so quickly in late 2020 and early 2021, in populations with little or no prior immunity to the virus.
They also found, however, that the more recent Delta and Omicron variants do not necessarily bind more strongly than the others, meaning that other processes must be considered when predicting which variants might become more prevalent.
Lipfert and colleagues say that their initial idea, early in the pandemic, was to use force spectroscopy to study how the coronavirus binds to cells. “In February and March 2020, we were wondering how our expertise in biophysics might help fight the global pandemic,” Lipfert explains. “While were we working on developing the first assay, which was detailed in a preprint in autumn 2020 and finally published in PNAS, the different variants-of-concern emerged and spread around the world. This naturally led us to ask the question as to whether our assay could also be used to probe for differences between the variants.”

Physicists simulate how SARS-CoV-2 forms
The team, which also includes scientists from LMU Munich and the Technical University of Munich, Stanford University, the University of Washington and Auburn University, hopes to use its assay and methodology to understand the effects of mutations in detail and even to predict new variants in the future. This could help us stay ahead of the virus by developing updated vaccines, they say.
“We would also like to use our method to test predicted and observed new variants of the coronavirus,” Lipfert tells Physics World. “In addition, we believe our approach could be very valuable for understanding host-pathogen interactions more generally.”
Their study is published in Nature Nanotechnology.